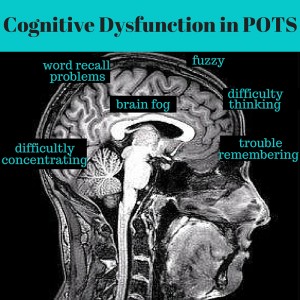
POTS is one of the most frequent forms of chronic orthostatic intolerance, and is a common source of disability among young adults. One of the most common symptoms reported by POTS patients is cognitive dysfunction or “brain fog.” These terms both indicate a loss of brain functioning in areas such as thinking, remembering, concentrating, and reasoning to a level that interferes with daily activities. In our center (Vanderbilt University’s Autonomic Dysfunction Clinic), approximately 80 to 90% of POTS patients report cognitive dysfunction and often describe it as: “difficulty thinking, concentrating, or paying attention; trouble remembering things; cloudy or fuzzy feeling in head; and having problems finding the right words.” This can occureven while patients are lying down or seated, which limits their ability to attend school or to work. While cognitive dysfunction is an almost universal finding in POTS patients, it is still poorly understood.
In response to our patient’s concerns, we designed a study to identify specific problem areas for cognitive function in POTS. We gave a series of standardized neuropsychological tests to POTS patients and compared their responses to healthy subjects matched for age and gender. We studied patients in the seated position, to minimize heart rate changes and related symptoms. We found clinically meaningful impairment in three areas of cognitive function in POTS patients. First, patients had impaired selective attention, or the ability to focus on specific stimuli when several stimuli are presented at the same time. For example, patients were slower and made more mistakes when asked to mark only the numbers 2 and 7 within a long series of numbers. Second, patients had impaired cognitive processing speed, indicating that it took longer to process information. Finally, patients had impaired executive function, indicating problems with planning, organizing information, and adapting to changes. There were no deficits in other areas of brain function including intelligence, memory, reaction time (psychomotor speed), and information retrieval from memory (verbal fluency). Importantly, in our study, there was no association between cognitive dysfunction and psychiatric symptoms such as mild depression or anxiety in POTS patients.
In summary, our study showed that POTS patients have deficits in specific areas of cognitive function including selective attention, processing speed, and executive function. These problems were observed even in the seated position. This may indicate that the cognitive dysfunction in POTS is not due to the increased heart rate and symptoms with standing, but rather may reflect part of the disease itself. Further studies are needed to determine the impact of standing, the underlying causes, and the optimal treatment strategies to manage this cognitive dysfunction.
Is cognitive dysfunction the same as brain fog?
There are several words that have been used to describe the cognitive dysfunction in POTS including brain fog, mental fog, mental fatigue, and mental clouding. These all refer to multiple symptoms that impair intellectual functioning to a level that interferes with daily activities. These symptoms can include difficulty thinking clearly, trouble concentrating or focusing, and mental confusion or lack of mental clarity.
What are the specific tests for cognitive function?
There is not a single test or series of tests used to diagnose cognitive dysfunction. Rather, there are numerous standardized neuropsychological tests that can provide information about different aspects of cognitive function. The basic purpose of these tests is to determine the likelihood of meaningful cognitive impairment, by comparing scores to normative values obtained from healthy subjects of similar age, gender, and education level. A potential limitation is that the tests may not have been validated in every population (such as POTS), and may have lower accuracy to detect changes in patients with mild levels of cognitive dysfunction.
Who can diagnose cognitive dysfunction?
A primary care physician can perform a general screening test for cognitive function, but this may not detect the more subtle changes that we found in POTS. In general, a neuropsychological evaluation is needed to gain a comprehensive understanding of how one’s brain is functioning. This involves a visit with a clinical neuropsychologist who will perform an interview and give a series of validated tests and questionnaires that look at a variety of brain functions such as intelligence, memory, attention, executive function, language, mood, and personality traits. The information from these tests may help in assessing brain function over time or after treatment.
What type(s) of cognitive dysfunction are common in POTS?
Our study showed problems with selective attention, cognitive processing speed, and executive function in POTS patients. Other studies have also shown problems with working memory, or the ability to hold onto and to process new and already-stored information, in POTS patients that also have chronic fatigue syndrome. This impairment in working memory may reflect the additional presence of chronic fatigue syndrome, as problems with memory and concentration have been well described in this patient population. It is important to note that there was a large variability in cognitive test scores in our study, with some POTS patients having scores within the normal range for healthy subjects. Thus, the diagnosis of cognitive dysfunction, and related treatment plans, should be considered on an individual basis.
What is the (suspected) cause of cognitive dysfunction in POTS?
The cause of cognitive dysfunction in POTS is still unknown. There have been several potential causes proposed. First, there is an association between elevated norepinephrine levels and psychiatric disorders such as depression, panic disorder, and attention deficit hyperactivity disorder. Since high levels of norepinephrine in the brain can disrupt cognitive function, it has been proposed that this mechanism could contribute to cognitive dysfunction in POTS patients with elevated norepinephrine levels (hyperadrenergic). We did not find an association between plasma norepinephrine levels and cognitive function in our study in POTS patients, but further studies are needed. Second, studies have shown that a reduction in brain blood flow may contribute to impaired memory in POTS patients with chronic fatigue syndrome. Finally, POTS patients often have other conditions including small fiber peripheral neuropathy, vasovagal syncope, immune system activation, pain, irritable bowel syndrome, and sleep disorders. These could all negatively impact cognitive function and overall mental health.
Is cognitive dysfunction similar to attention deficit hyperactivity disorder (ADHD)? Is using ADHD medication to combat cognitive dysfunction recommended in POTS?
In a previous study, we compared the psychiatric profile of POTS patients to adult patients with ADHD (Vidya Raj and colleagues, Journal of Neurology, Neurosurgery & Psychiatry, 2009). We showed that people with both disorders have difficulty maintaining attention, but that it is more severe in ADHD. Furthermore, POTS patients developed problems with attention later in life and did not show significant hyperactivity, which is opposite to the childhood presence and the common feature of hyperactivity with ADHD. Therefore, the pattern of cognitive dysfunction appears to be different in POTS versus ADHD. The most common treatment for ADHD is the use of stimulants (such as Adderall and Ritalin) to enhance alertness, attention, and memory. There is no information on the effectiveness of ADHD medications in POTS. To address this, we are currently conducting a study examining the effects of the stimulant drug modafinil on cognitive function in POTS patients at the Vanderbilt Autonomic Dysfunction Center. Since there is concern that stimulants could worsen heart rate control in POTS, we are also examining the effect of modafinil in combination with the beta-blocker propranolol. This is the first study addressing treatment strategies to manage cognitive dysfunction in POTS.
![AmyA[1]](https://dysautonomiainternational.org/blog/wordpress/wp-content/uploads/2016/02/AmyA1.jpg) Guest author Amy Arnold, PhD, is a Research Instructor in the Division of Clinical Pharmacology at the Vanderbilt University School of Medicine. She is also a member of the Vanderbilt Autonomic Dysfunction Center. Her clinical research program focuses on understanding the causes of autonomic nervous system disorders such as POTS and autonomic failure, as well as new treatment strategies for these conditions.
Guest author Amy Arnold, PhD, is a Research Instructor in the Division of Clinical Pharmacology at the Vanderbilt University School of Medicine. She is also a member of the Vanderbilt Autonomic Dysfunction Center. Her clinical research program focuses on understanding the causes of autonomic nervous system disorders such as POTS and autonomic failure, as well as new treatment strategies for these conditions.