Sjogren’s is the second most common cause of autonomic neuropathy, and April is Sjogren’s Awareness Month, so we invited guest blogger Sarah Schafer, MD to share some information on Sjogren’s for the dysautonomia community.
Your dysautonomia may be caused by Sjogren’s disease.
Here’s why that matters.
I’m a medical doctor with POTS and Sjogren’s disease. It took years to get diagnosed, and I’m determined to make sure no one else goes through the ordeal I’ve had to endure.
I’ve had symptoms of both postural orthostatic tachycardia syndrome (POTS) and Sjogren’s since I was a teenager. Though I felt increasingly unwell as I aged, I remained able to function until a sudden decline at 44, when extreme fatigue, lightheadedness, and other symptoms left me mostly bedridden. I lost my career, my ability to do things with my children, and almost everything else I loved to do.
This was the early 2000s. My doctors never considered Sjogren’s, even though I had classic symptoms, including 25 years of specialty treatment for severe dry eyes. Neither they nor I knew much about Sjogren’s, and none of us had heard of POTS.
After a year of normal tests, my doctors started downplaying my symptoms as being caused by stress or depression. I wasn’t depressed. My symptoms weren’t caused by stress; they were caused by Sjogren’s and POTS. I was stressed because I was severely ill and unable to get a proper diagnosis and care.
Even though I’m a doctor, I encountered the same dismissal and psychologization of my symptoms that many women face when doctors can’t find a diagnosis. Fortunately, my medical knowledge enabled me to research scientific literature, which helped me figure out that I likely had Sjogren’s and POTS. I then used my research to advocate with my doctors for a Sjogren’s diagnosis, and later, to educate them about POTS.
Although treatments have helped somewhat, they came too late for me to have the quality of life I could have had with earlier intervention.
What is Sjogren’s disease?
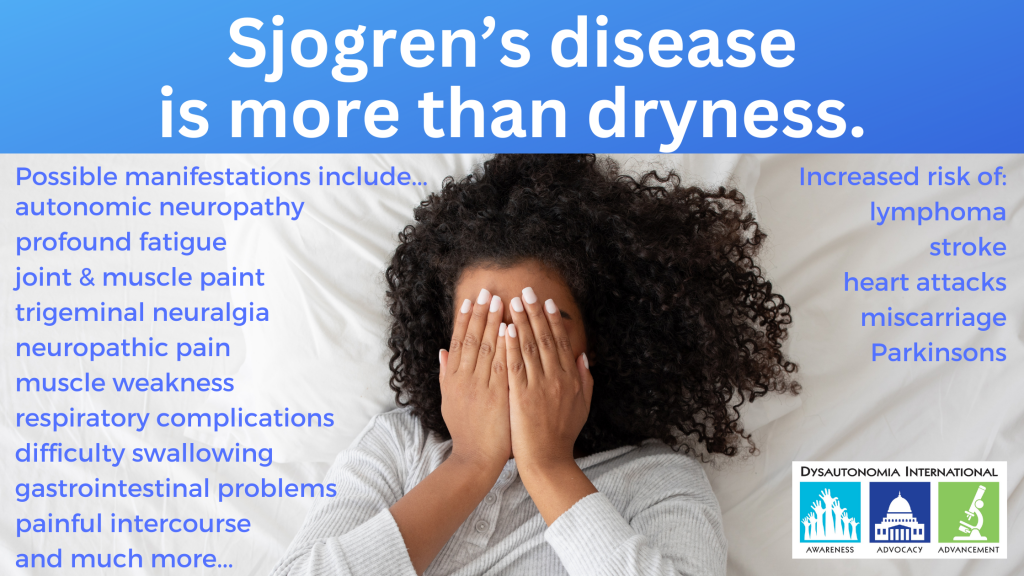
Sjogren’s is a serious autoimmune rheumatic disease that affects many body systems. Sjogren’s is never just dry eye and dry mouth, even though that is how it was originally described.
Sjogren’s disease is a common cause of dysautonomia.
Most people with Sjogren’s disease have dysautonomia, which can cause a multitude of conditions such as POTS, orthostatic hypotension (OH), stomach, gut, and bladder problems, and unusual sweating. But most doctors don’t know much about dysautonomia and don’t realize that many symptoms of Sjogren’s disease are related to dysautonomia. If you have dysautonomia, you might also have Sjogren’s.
Why is it important to know if you have Sjogren’s?
Sjogren’s is a complex and unpredictable disease that frequently leads to a significant decline in quality of life, mainly related to fatigue and pain, not dryness. In some instances, especially if it’s not diagnosed and monitored closely, Sjogren’s can be life-threatening.
Sjogren’s disease can damage nerves, organs, and joints, sometimes without producing obvious symptoms. The only way to detect this silent damage is by monitoring Sjogren’s patients for a wide range of systemic manifestations. Early detection of systemic (non-dryness) manifestations allows for timely intervention, when treatments are most likely to be effective. Contrary to what some doctors may tell you, there are treatments that help slow the progression of Sjogren’s disease, make you feel better, and sometimes even save your life.
Early symptoms of Sjogren’s disease
Sjogren’s affects everyone differently. While doctors are taught to look for dry eyes and mouth as signs of Sjogren’s, most people seek a diagnosis because of other symptoms like fatigue, cognitive problems, and pain, not dryness. And dry eyes and mouth aren’t always present, especially in people with neurological problems like dysautonomia.
Doctors often overlook lightheadedness (due to POTS or OH) and painful neuropathy as early Sjogren’s symptoms. Other common early symptoms include severe fatigue, widespread pain, cognitive dysfunction (or “brain fog”), severe headaches, difficulty swallowing or digesting, joint and muscle pain, a persistent cough, shortness of breath, and Raynaud’s phenomenon.
It’s possible to have many of these symptoms, or none of them. Since most doctors aren’t trained to recognize all the different ways Sjogren’s can show up in the body, they frequently mistake it for fibromyalgia, irritable bowel syndrome, anxiety, or functional neurological disorder (FND).
Why is Sjogren’s diagnosis missed or late?
Extreme delays in Sjogren’s diagnosis are common because clinicians receive minimal education about Sjogren’s disease. The limited information they’re provided is often inaccurate and outdated. Many medical educators perpetuate the misconception that Sjogren’s is a rare, unimportant dryness syndrome, primarily affecting middle-aged women.
The reality is that:
- Sjogren’s is common, not rare. Sjogren’s disease affects approximately 1 in 100 people in the US (most cases are undiagnosed), similar to the prevalence of rheumatoid arthritis (RA) and three times that of lupus. RA and lupus are closely related diseases that receive far more attention than Sjogren’s disease.
- While many people with Sjogren’s disease experience dry eyes and mouth, there is no dryness-only version of Sjogren’s.
- Although 9 out of 10 Sjogren’s patients are women, Sjogren’s can affect anyone, at any age, including men and children.
- Sjogren’s often begins in childhood or early adulthood, but diagnosis is frequently delayed for decades, when the disease has caused significant damage and symptoms become unmanageable.
Sjogren’s diagnosis: what you need to know.
If you think you might have Sjogren’s, talk to your doctor about testing. Getting a diagnosis can take time, especially if your blood tests for SSA and SSB are negative, which is common in people with Sjogren’s and dysautonomia.
You may need to learn a lot about Sjogren’s and be your own advocate to get diagnosed and treated properly. Many doctors only know about dryness and may not know which tests to use. Some rheumatologists misuse classification criteria as a rigid checklist, leaving many people living with Sjogren’s undiagnosed, unmonitored, and untreated. I founded my website, Sjogren’s Advocate, to give patients the tools and strategies they need to advocate for themselves when they encounter barriers to diagnosis and care.
Hope is on the horizon.
New treatments for systemic manifestations, expected soon, should raise awareness among doctors that Sjogren’s is not a rare, unimportant dryness syndrome primarily affecting middle-aged women. Even if these new medications aren’t a good fit for every patient, the increased visibility of Sjogren’s will hopefully improve diagnosis and care. Until medical education catches up to the realities of Sjogren’s disease, self-advocacy remains key.
Guest blogger Dr. Sarah Schafer founded Sjogren’s Advocate in 2018 as part of her mission to improve patient awareness and care. The Sjogren’s Advocate website is a great resource for anyone who is looking for more information on Sjogren’s.
_____________
Interested in learning more about Sjogren’s? Check out these Dysautonomia International educational videos.
Dysautonomia International President Lauren Stiles and Patient Advisory Board Chair Jennifer Samghabadi, F-NP, and Dr. Sarah Schafer from Sjogren’s Advocate share what dysautonomia patients need to know about SJogren’s and discuss their own experience with POTS and Sjogren’s.
Dysautonomia International Medical Advisory Board member Dr. Brent Goodman presented this lecture on Sjogren’s at our Dysautonomia International’s 2019 Conference.