by Dr. Svetlana Blitshteyn
Since POTS affects predominantly women of reproductive age, it is not surprising that at some point after the diagnosis of POTS, questions about the safety of pregnancy will be raised. As a POTS specialist, I am often asked these questions by women in their 20s, 30s and sometimes 40s. When women and their partners are ready for family planning, a chronic illness like POTS can make simple decisions difficult and difficult decisions even more challenging.
The good news is that POTS does not need to steal your dream of becoming a mother as many women with POTS have had successful pregnancies. Still, the course of POTS during pregnancy appears to be variable – i.e. 60-70% of patients will experience improved symptoms of POTS during pregnancy, while 30-40% will feel worse (1,2). Thus, women who are diagnosed with POTS and wish to become pregnant will need to educate themselves, and probably their obstetrician, regarding the course of POTS during and after pregnancy and possible complications that may arise along the way.
Typically, I advise women with POTS who want children to get pregnant sooner rather than later. This is because when you add advanced maternal age (defined as 35 years and older), to the pre-existing medical condition, the odds of developing various pregnancy and fetal complications become higher than if pregnancy occurs at a younger age.
There may be a possibly higher miscarriage rate in women with POTS, which may make it more difficult and/or take longer to conceive. Additionally, a study from Vanderbilt University suggested that there may be a higher rate of gynecological disorders in women with POTS, such as endometriosis and uterine fibroids (3). Thus, for women with POTS who wish to get pregnant, several issues may arise that would require a careful and comprehensive approach on the part of the POTS specialist, gynecologist and the patient, in making pregnancy a priority. Below are the answers to common questions raised by POTS patients regarding pregnancy.
1. Is pregnancy safe for POTS patients?
Generally, there are no contraindications to pregnancy in patients with POTS. However, since POTS is a disorder that has many underlying causes, many of which are still unknown, every patient with a diagnosis of POTS will need to ask that question to their POTS specialist. If you have mild symptoms or your POTS is fairly well-controlled, the decision of whether it is safe to undertake pregnancy will be easier to make. However, even for women with severe POTS who want to become pregnant, pregnancy is still not contraindicated, although it may require multiple specialists, various interventions and careful planning for labor, delivery and the postpartum period.
2. Are there pregnancy complications that are more likely to occur in POTS patients?
In my study on POTS and pregnancy, almost 60% of women reported severe vomiting or hyperemesis gravidarum (extreme and persistent vomiting during pregnancy) and 40% of women experienced fatigue during pregnancy (1). Other common POTS symptoms during pregnancy were presyncope and tachycardia. Also noteworthy is that there was a higher rate of miscarriage in patients with POTS compared to the general population. The good news is that there were no maternal or fetal complications attributable to POTS, as far as we know. However, a number of questions still remain and need to be studied further. These questions include whether there is an increased risk of pre-eclampsia, pregnancy-induced hypertension or postpartum hypertension in women with POTS; whether a subsequent pregnancy results in worse symptomatic exacerbation than the first pregnancy, and what the course and outcomes are in women with postpartum onset of POTS who become pregnant again.
3. Does pregnancy make POTS symptoms worse or trigger a relapse after delivery?
In our study, about 50% of women with pre-existing POTS felt better or stable 6 months postpartum, compared to before pregnancy (1). In a study by Dr. Blair Grubb, about 30% of women felt worse after giving birth (with the postpartum period not defined), while 70% of women reported “stable” symptoms (2). In the study by Mayo Clinic, there were no differences in the autonomic function tests scores in women with POTS who had children compared to women with POTS who did not (4). In conclusion, about 30-50% of women with pre-existing POTS reported worsening of symptoms after giving birth. Furthermore, for a number of healthy women, pregnancy can trigger a new-onset POTS, and for substantial proportion of women with pre-existing POTS, pregnancy will be an exacerbating factor. Conversely, about half of women with POTS can expect no change in their symptoms after the pregnancy.
4. What POTS medications are safe to take during pregnancy?
While there are no pregnancy “Class A” medications (i.e., the FDA classification for the safest drugs for pregnant women) available to treat POTS, in our study women who used medications, if necessary, to control symptoms, did not have any adverse maternal or fetal effects. I have used a low dose of a beta blocker to control tachycardia and other symptoms in pregnant patients with POTS safely. Florinef and Mestinon can also be continued during pregnancy if necessary, but we have less experience with midodrine during pregnancy since it’s a newer medication. There is also an option to continue or switch to Prozac in those women who take SSRIs before pregnancy. Medications that need to be weaned off or used only under special circumstances and/or sparingly are benzodiazepines, like clonazepam, Ativan and Xanax, and stimulants, such as Ritalin and Adderall.
5. What POTS medications must be stopped before pregnancy and for how long?
Ideally, all medications would have to be stopped prior to conception. However, for many women with POTS and other chronic illnesses, this would be an unrealistic goal. If at all possible, medications during the 1st trimester when the fetus is developing, should be avoided. If this is not possible, as will be the case in many patients, the lowest dose of the medication should be used. I recommend weaning off benzodiazepines and stimulants such as Ritalin and Adderall slowly, under the supervision of your physician, before planning to conceive. If pregnancy is unplanned, there may be a faster weaning schedule to discontinue controlled substances. It might be beneficial to consult a high risk obstetrician, a.k.a maternal-fetal medicine specialist, before you plan to become pregnant with a chronic illness, in addition to your POTS specialist.
6. Does having POTS pose any risks for the baby in utero and postpartum?
All four studies on POTS and pregnancy conclude that there appears to be no negative effects on the fetus or the child secondary to the maternal POTS (1,2,4,5), and this is a reassuring conclusion. I am often asked if fainting can harm the baby, and the answer is no, a simple isolated faint will typically not harm the fetus because the fetus is protected by the surrounding amniotic fluid. However, if syncope during pregnancy becomes frequent and persistent, this may affect placental blood flow to the baby and will likely require an intervention from your doctor to effectively manage recurrent syncope.
7. Do any of the common POTS medications pass through to breast milk?
It is well-established that breast milk is superior to any formula for the baby. Yes, a small percentage of the medication will be excreted in the breast milk, but more likely than not, it would not affect the newborn. Some beta blockers are noted to be safer in breastfeeding than others. For example, metoprolol is considered safer than atenolol because atenolol has a longer half-life. Additionally, Prozac, which is acceptable during pregnancy, may be more harmful to the newborn through breastfeeding than Zoloft. Once again, the lowest dose of the medication with the least potential for the adverse effects for the baby would be utilized. Your pediatrician and pharmacist would be the best specialists to answer questions regarding specific medications and breastfeeding.
It is also important to mention that some women may be unable to breastfeed at all for various reasons. The medical community and our society strongly emphasize the benefits of breastfeeding and breast milk, which may lead to feelings of anxiety, depression, guilt and low self-esteem in those women who are unable to breastfeed their baby. I want to reassure those women that your baby will also thrive with bottle-feeding and formula. It would be more important for both the mother and the baby to be healthy and thriving, regardless of the mode and type of feeding.
8. Will my child develop POTS?
POTS is not a genetic disorder in the sense that it does not follow the type of genetic transmission that occurs in cystic fibrosis, for example. Although research in the genetics of POTS is currently lacking, it has been shown in various studies that POTS may run in families (13% to 40% of patients) (1). While POTS is not transmissible to children through one particular gene, it is possible that children may be predisposed to autonomic dysfunction as adolescents or adults through their overall genetic makeup. However, at this time, it is impossible to predict or calculate the likelihood of a child developing POTS if one parent is affected.
In summary, while POTS, like many chronic illnesses, is a concern to women who wish to become pregnant, the research studies available to date are reassuring that women with POTS may safely undertake pregnancy if they choose to do so. While there may be additional risks and complications, such as a possible increase in miscarriage rate and hyperemesis gravidarum, overall there appears to be no adverse maternal or fetal complications attributable to POTS. Nevertheless, there will be a significant number of women (about 50%), whose symptoms of POTS will become worse after pregnancy, and to this end, having a good support system and help with childcare are essential to the well-being of the mother, the baby and other family members.
References
1. Blitshteyn S, Bett GL, Poya H. Pregnancy in Postural Tachycardia Syndrome: clinical course and maternal and fetal outcomes. J Matern Fetal Neonatal Med. 2012; 25: 1631-1634.
2. Kanjwal KK, Karabin B, Grubb BP. Outcomes of pregnancy in patients with Postural Orthostatic Tachycardia Syndrome. PACE 2009; 32:1000-1003.
3. Peggs, KJ, Nguen H, Enayat D, et al., Gynecologic disorders and menstrual cycle lightheadedness in postural tachycardia syndrome. Int J Gynaecol Obstet. 2012; 118: 242-246.
4. Kimpinski K, Iodice V, Sandroni P, Low PA. Effect of pregnancy on Postural Tachycardia Syndrome. Mayo Clin Proc 2010; 85: 639-644.
5. Powless CA, Harms RW, Watson WJ. Postural tachycardia syndrome complicating pregnancy. J Matern Fetal Neonatal Med 2010; 23: 850-853.
 Guest author Svetlana Blitshteyn, MD is the Director of the Dysautonomia Clinic and a Clinical Assistant Professor of Neurology at the University at Buffalo School of Medicine and Biomedical Sciences. She also serves as a volunteer on Dysautonomia International’s Medical Advisory Board.
Guest author Svetlana Blitshteyn, MD is the Director of the Dysautonomia Clinic and a Clinical Assistant Professor of Neurology at the University at Buffalo School of Medicine and Biomedical Sciences. She also serves as a volunteer on Dysautonomia International’s Medical Advisory Board.















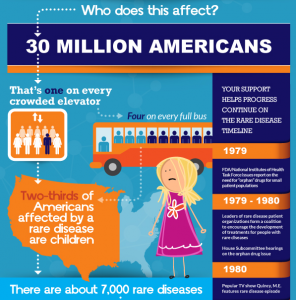
 Dysautonomia International is pleased to partner with the National Organization for Rare Disorders (NORD) to celebrate Rare Disease Day today. Did you know that overall, rare diseases are not that rare?
Dysautonomia International is pleased to partner with the National Organization for Rare Disorders (NORD) to celebrate Rare Disease Day today. Did you know that overall, rare diseases are not that rare?