“If we want an answer from nature, we must put our questions in acts, not words, and the acts may take us to curious places. Some questions were answered in the laboratory, others in mines, others in a hospital where a surgeon pushed tubes in my arteries to get blood samples, others on top of Pike’s Peak in the Rocky Mountains, or in a diving dress on the bottom of the sea. That is one of the things I like about scientific research. You never know where it will take you next.” — J.B.S. Haldane
From essay ‘Some Adventures of a Biologist’, as quoted in Ruth Moore, Man, Time, And Fossils (1953), 174
While not dressed as suggested by Dr. Haldane, I recently joined a massive expedition
intent on making new scientific discoveries. Working with an international group of
colleagues, I screened blood samples from 113 Swedish individuals with POTS and 283
people who don’t have POTS (controls) in search of one or more biomarkers.
Biomarkers are molecules present in a biological sample at concentrations that are
clearly different between patients and healthy people. Ideally, a biomarker would also
be more abnormal in more severe disease states, and closer to normal as a patient’s
symptoms improved or went in remission. In this particular case, we were hoping to
identify a biomarker that is as reliable and specific as the tilt test for identifying POTS,
so that someday, perhaps, POTS can be diagnosed by a blood test rather than the tilt
test. We used a new testing approach called Proximity Extension Assay, which allows
us to measure concentrations of 57 human protein biomarkers in a single sample
thanks to new DNA technology.
So, did we catch anything? The answer is yes, although we are still trying to puzzle out
the implications. We found one protein that was significantly less common in the blood
of POTS patients than in the blood of controls – furin. This protein was found in much
lower concentrations in POTS patients than in controls, but was also less abundant in
the blood of POTS patients with more severe POTS on tilt testing than in those with
milder POTS.
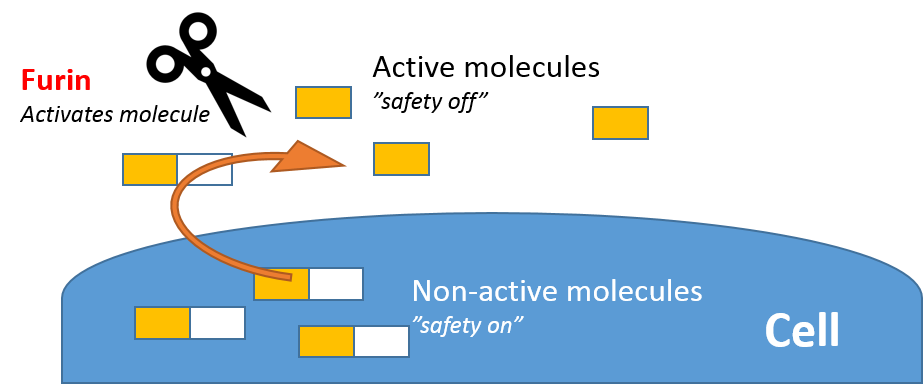
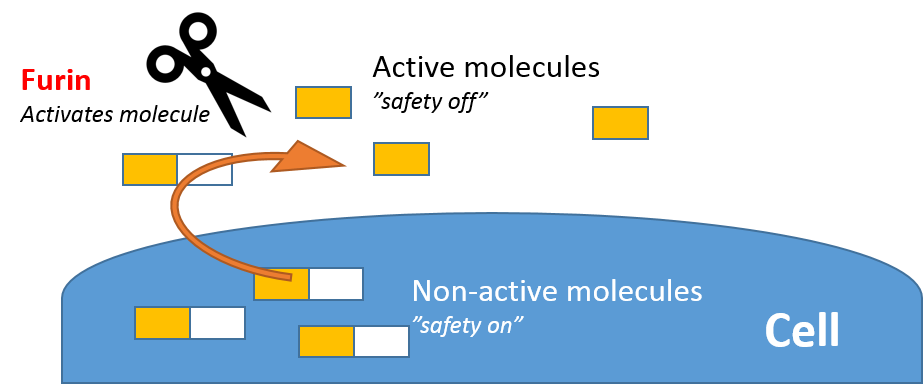
Furin promotes the maturation of secreted chemical messengers at the cell surface.
Furin is found throughout the body and has been reported to process a large number of
cytokines and chemokines, including anti-inflammatory transforming growth factor
(TGF)-β1 and pro-inflammatory secreted TNF-family members. Cytokines and
chemokines play important roles in the immune system.
Interestingly, previous evidence has suggested that inhibition of furin may result in a
breakdown of peripheral immune tolerance (Pesu et al., 2008) and development of
systemic autoimmune disease (Lisi et al., 2010). Recent findings report low furin levels
correlate to worsening systemic disease activity in Sjögren’s syndrome (Ranta et al.,
2018). It is important to note that only one POTS patient in our series had a confirmed
autoimmune disease, so there is much we still have to learn about the immune system
in POTS.
So how does this help us diagnose and treat POTS? Well, if our findings are replicated
in other populations, a furin blood test may assist in diagnosing POTS in the future. It
may also be that POTS patients with a very low furin may respond in a different way to
certain treatments than do those with more normal levels of furin. There is much
research to be done exploring why POTS patients have low furin levels, and how this
impacts their immune system.
As said so well by Dr. Haldane, “If we want an answer from nature, we must put our
questions in acts, not words…”! This is what I intend to do, continuing now from the
bottom of the sea to the next curious place. Stay tuned!
 Guest blogger Jonas Axelsson, MD, PhD is the Director of the Center for Apheresis and Stem Cell Handling and an Associate Professor of Renal Medicine at the Karolinska Institutet in Sweden. He is interested in studying the immune system in POTS, ME/CFS and other conditions. He will be a guest speaker at the Dysautonomia International 7th Annual Conference this summer, where he will also be conducting a research study exploring even more immune and genetic biomarkers in POTS. When he’s not trying to figure out complicated diseases in the lab, he enjoys sailing, diving and photography.
Guest blogger Jonas Axelsson, MD, PhD is the Director of the Center for Apheresis and Stem Cell Handling and an Associate Professor of Renal Medicine at the Karolinska Institutet in Sweden. He is interested in studying the immune system in POTS, ME/CFS and other conditions. He will be a guest speaker at the Dysautonomia International 7th Annual Conference this summer, where he will also be conducting a research study exploring even more immune and genetic biomarkers in POTS. When he’s not trying to figure out complicated diseases in the lab, he enjoys sailing, diving and photography.
REFERENCES
Spahic, J., Ricci, F., Aung, N., Axelsson, J., Melander, O., Sutton, R., Hamrefors, V., and Fedorowski, A. Proconvertase Furin Is Downregulated in Postural Orthostatic Tachycardia Syndrome. Front. Neurosci., 29 March 2019. doi.org/10.3389/fnins.2019.00301
PubMed Abstract | CrossRef Full Text | Google Scholar
Pesu, M., Watford, W. T., Wei, L., Xu, L., Fuss, I., Strober, W., et al. (2008). T-cell-expressed proprotein convertase furin is essential for maintenance of peripheral immune tolerance. Nature 455, 246–250. doi: 10.1038/nature07210
PubMed Abstract | CrossRef Full Text | Google Scholar
Lisi, S., Sisto, M., Lofrumento, D. D., Cucci, L., Frassanito, M. A., Mitolo, V., et al. (2010). Pro-inflammatory role of Anti-Ro/SSA autoantibodies through the activation of Furin-TACE-amphiregulin axis. J. Autoimmun. 35, 160–170. doi: 10.1016/j.jaut.2010.06.020
PubMed Abstract | CrossRef Full Text | Google Scholar
Ranta, N., Valli, A., Gronholm, A., Silvennoinen, O., Isomaki, P., Pesu, M., et al. (2018). Proprotein convertase enzyme FURIN is upregulated in primary Sjogren’s syndrome.Clin. Exp. Rheumatol. 36(Suppl. 112), 47–50.
Google Scholar
Piguet, V., Wan, L., Borel, C., Mangasarian, A., Demaurex, N., Thomas, G., et al. (2000). HIV-1 Nef protein binds to the cellular protein PACS-1 to downregulate class I major histocompatibility complexes. Nat. Cell. Biol. 2, 163–167. doi: 10.1038/35004038
PubMed Abstract | CrossRef Full Text | Google Scholar
Guimont, P., Grondin, F., and Dubois, C. M. (2007). Sox9-dependent transcriptional regulation of the proprotein convertase furin. Am. J. Physiol. Cell Physiol. 293, C172–C183. doi: 10.1152/ajpcell.00349.2006
PubMed Abstract | CrossRef Full Text | Google Scholar




 by
by 





 by
by 
 Robin and Hannah Lucas are a mother-daughter duo from Georgia who are very active in the dysautonomia community. They have been volunteers for Dysautonomia International for two years and Robin helps lead Dysautonomia International’s Georgia Support Group.
Robin and Hannah Lucas are a mother-daughter duo from Georgia who are very active in the dysautonomia community. They have been volunteers for Dysautonomia International for two years and Robin helps lead Dysautonomia International’s Georgia Support Group.